Human Papillomavirus, or HPV, is one of the most common sexually transmitted diseases. This viral infection can cause genital warts and even cervical cancer in women.
What exactly is HPV? What are its symptoms, causes, and how is it treated? Here’s a comprehensive explanation.
What is HPV?
HPV is a group of viruses consisting of more than 200 different strains or types. The viruses infect skin and mucous membrane cells, mainly in the genital area, anus, mouth, and throat.
Some types of HPV can cause warts, while others can trigger cancer, especially cervical cancer in women.
Almost everyone who is sexually active will be exposed to HPV at some point in their lives. However, most HPV infections do not cause symptoms and resolve on their own.
Symptoms of HPV
Most HPV infections do not cause symptoms or health problems. When symptoms do appear, they depend on the type of HPV causing the infection.
Symptoms of low-risk HPV include:
- Genital warts (condyloma acuminata): small, cauliflower-shaped bumps in the genital area, usually painless. These warts can appear weeks to months after HPV infection.
- Common warts: rough bumps that usually appear on hands and feet.
- Plantar warts: hard, rough wart-like growths on the soles of the feet that can cause pain when walking or standing.
- Flat warts: smaller flat-topped growths, usually on the face, neck, or under the chin, and often occurring in children.
Meanwhile, symptoms of high-risk HPV are generally absent until it develops into cancer. Symptoms of HPV-related cancers may include:
- Abnormal vaginal bleeding, bleeding after sexual intercourse, or postmenopausal bleeding (cervical cancer)
- Anal bleeding, pain, itching, or lumps (anal cancer)
- Hoarseness or persistent voice changes (throat cancer)
- Mouth or tongue sores that don’t heal (oral cancer)
- Lumps in the groin or swollen groin (vulvar cancer)
It’s important to remember that most HPV infections do not cause symptoms. That’s why routine screenings like Pap smears are crucial for early detection of cervical cancer.
Causes of HPV
HPV spreads through skin-to-skin contact, usually during sexual activity, including vaginal, anal, and oral sex. HPV can also be transmitted through intimate skin-to-skin contact without penetration.
HPV transmission can occur when infected skin comes into contact with a partner’s skin. This can happen even when the infected person shows no signs or symptoms. HPV infections are very common, and most people get them after becoming sexually active.
Additionally, a mother infected with HPV risks transmitting it to her baby during childbirth, although this is rare. When it does occur, the baby may develop warts in the respiratory tract.
Most HPV infections resolve on their own within 1-2 years without causing health problems. Persistent infections with high-risk types of HPV can lead to abnormal cell changes that may develop into cancer if not detected and treated.
Risk Factors for HPV
Factors that can increase the risk of contracting HPV include:
- Having multiple sexual partners. The more sexual partners you have, the greater the risk of HPV infection.
- Having a sexual partner who also has multiple sexual partners or is infected with HPV.
- Engaging in sexual activity at a young age. HPV infections are more common in teenagers and young adults, especially those who become sexually active before the age of 18.
- Having a weakened immune system due to medical conditions such as HIV/AIDS or medications that suppress the immune system.
- Smokers are more likely to develop genital warts and HPV-related cervical cancer compared to non-smokers.
- Family history of cervical cancer. Having a mother or sister with cervical cancer increases your risk.
Although these factors can increase the risk, anyone who is sexually active is at risk of HPV infection. That’s why HPV vaccines and routine cervical cancer screenings are recommended to reduce risk.
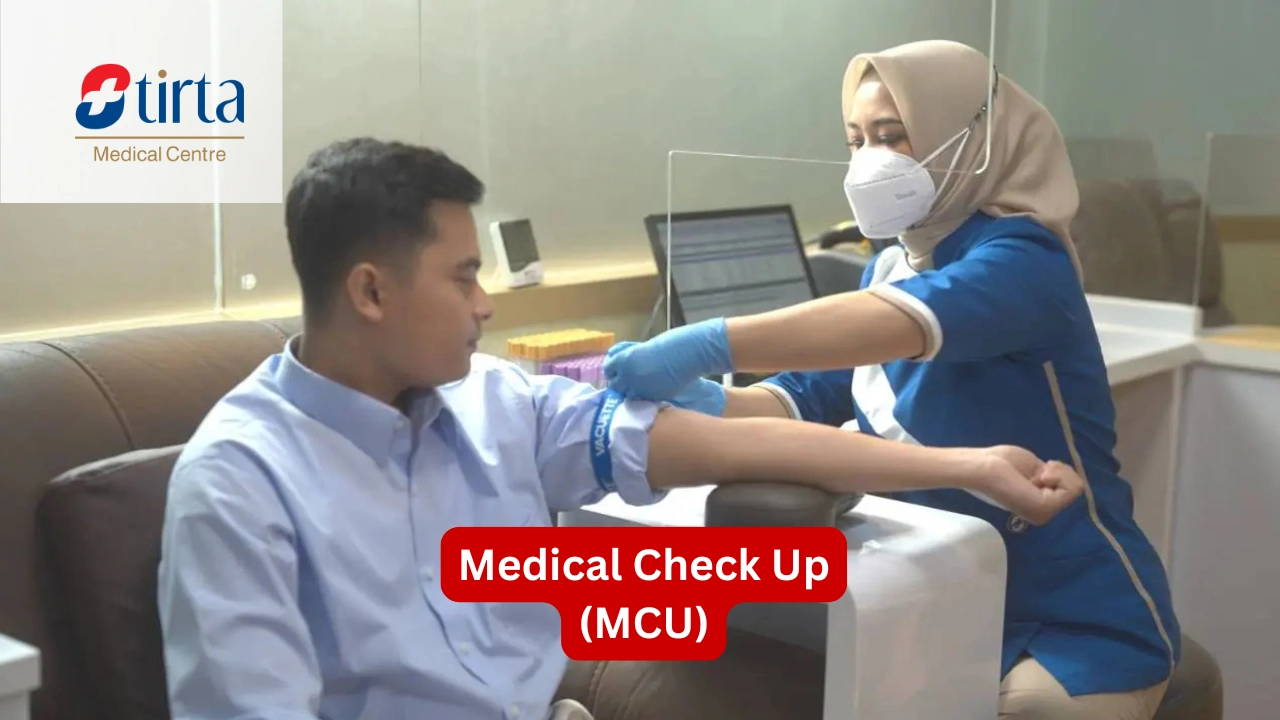
Diagnosis of HPV
For visible genital warts, doctors can usually diagnose them through visual examination. If the results are unclear, the doctor may take a biopsy (tissue sample) from the wart for laboratory examination.
For high-risk HPV, available screening tests include:
1. Pap smear
A procedure where the doctor collects cells from the cervix to be examined under a microscope. Pap smears are recommended for women aged 21-65 every 3 years.
2. HPV test
This test detects high-risk HPV DNA in cervical cell samples. The HPV test can be done alongside a Pap smear. It’s recommended for women over 30 years old every 5 years.
3. Colposcopy
If a Pap smear or HPV test is abnormal, the doctor may recommend a colposcopy, where the cervix is examined using a magnifying instrument (colposcope). The doctor may take biopsy samples from suspicious areas.
For men, there is currently no approved screening test for detecting HPV infection. However, some doctors may offer anal examinations for men who have sex with men and are at high risk for anal cancer.
It’s important to remember that a positive HPV test doesn’t always mean someone will get cancer. It only means that additional precautions and monitoring may be necessary.
Treatment of HPV
There is no cure for HPV infection. However, the immune system can usually clear HPV infection on its own within 1-2 years. During this time, regular screening for changes in cervical or anal canal cells is recommended.
For genital warts caused by low-risk HPV, several treatment options include:
- Topical prescription creams or solutions such as podofilox (Condylox), imiquimod (Aldara, Zyclara), and sinecatechins (Veregen)
- Cryotherapy
- Electrocautery
- Laser therapy
- Surgical excision
Treatment options depend on the size, location, and number of warts. Often, a combination of several methods is necessary.
Treatment can cause discomfort and may require multiple sessions. Even if warts disappear, HPV infection may still be present and transmissible.
Precancerous lesions and cancers associated with high-risk HPV are usually treated in the same way as non-HPV precancerous lesions and cancers in the same body location. This may involve surgical excision, radiotherapy, and/or chemotherapy depending on the stage, location, and other patient factors.
It’s important to undergo routine screening and follow up on abnormal results for early detection and treatment of cell changes that may develop into cancer.
HPV Complications
Although HPV infections often do not cause symptoms and can resolve on their own, some types of HPV can lead to severe problems if not treated.
Here are some of the main complications that can be caused by HPV:
– Cervical Cancer
One of the most serious complications of HPV is cervical cancer. Most cervical cancer cases are caused by long-lasting HPV infection, particularly high-risk types like HPV 16 and 18.
These viral infections can cause pre-cancerous changes in cervical cells, which, if left untreated, can develop into cervical cancer.
– Other Cancers
In addition to cervical cancer, HPV is also associated with other types of cancer, including:
- Vulvar cancer
- Vaginal cancer
- Penile cancer
- Anal cancer
- Oropharyngeal cancer (mouth and throat cancer)
Although these cancers are rarer than cervical cancer, HPV infection remains a major risk factor for their development.
– Genital Warts
Some low-risk HPV types, especially HPV 6 and 11, can cause genital warts. Genital warts are small, cauliflower-like skin growths in the genital area.
Although genital warts are usually harmless, they can cause physical discomfort and emotional distress. Genital warts are also highly contagious and can be transmitted through sexual contact.
– Recurrent Respiratory Papillomatosis (RRP)
RRP is a rare condition characterized by the growth of warts in the larynx (voice box), trachea (windpipe), or lungs. This condition most often occurs in children who have been exposed to HPV types 6 or 11 during childbirth.
RRP can cause hoarseness, difficulty breathing, and in severe cases, airway obstruction.
Prevention of HPV
Steps that can help prevent HPV infection include:
- Getting the HPV vaccine. The HPV vaccine is available for men and women aged 11-45 years.
- Using latex barriers, such as condoms and dental dams during sex. These can reduce the risk, but HPV can still be transmitted through skin-to-skin contact.
- Limiting the number of sexual partners. The more sexual partners, the greater the likelihood of exposure to HPV.
- Getting regular cervical cancer screenings. Pap smear and HPV tests can help detect cervical changes before they develop into cancer.
- Not smoking.
Knowing the risk factors and taking preventive measures can help reduce the risk of getting HPV and its complications.
If you have concerns related to HPV, you can prevent HPV infection at Tirta Medical Centre (TMC), which provides HPV vaccines that can be administered at all Tirta branches throughout Indonesia or at your home (home care).
References:
- Mayo Clinic. Accessed in 2024. HPV infection – Symptoms & causes: https://www.mayoclinic.org/diseases-conditions/hpv-infection/symptoms-causes/syc-20351596
- WebMD. Accessed in 2024. Information About Human Papillomavirus (HPV): https://www.webmd.com/sexual-conditions/hpv-genital-warts/hpv-virus-information-about-human-papillomavirus
- CDC. Accessed in 2024. About Genital HPV Infection: https://www.cdc.gov/sti/about/about-genital-hpv-infection.html
- Cleveland Clinic. Accessed in 2024. HPV (Human Papillomavirus): Causes, Symptoms & Treatment: https://my.clevelandclinic.org/health/diseases/11901-hpv-human-papilloma-virus
- NHS. Accessed in 2024. Human papillomavirus (HPV): https://www.nhs.uk/conditions/human-papilloma-virus-hpv/
- Medical News Today. Accessed in 2024. Human papillomavirus (HPV): Treatment, symptoms, and causes: https://www.medicalnewstoday.com/articles/246670
- Healthline. Accessed in 2024. Human Papillomavirus Infection: Symptoms and Prevention: https://www.healthline.com/health/human-papillomavirus-infection
- National Cancer Institute. Accessed in 2024. Cervical Cancer Causes, Risk Factors, and Prevention: https://www.cancer.gov/types/cervical/causes-risk-prevention
- Mayo Clinic. Accessed in 2024. HPV infection – Diagnosis & treatment: https://www.mayoclinic.org/diseases-conditions/hpv-infection/diagnosis-treatment/drc-20351602
- The New Zealand HPV Project. Accessed in 2024. HPV Diagnosis & Detection: https://www.hpv.org.nz/hpv-diagnosis
- Everlywell. Accessed in 2024. HPV Complications: What Are The Complications Of HPV?: https://www.everlywell.com/blog/hpv/hpv-complications/
- Cleveland Clinic. Accessed in 2024. Anal Warts (Condyloma): Treatment, Symptoms & Causes: https://my.clevelandclinic.org/health/diseases/24097-anal-warts